Participants
- Eelco de Koning
- Françoise Carlotti
- Bahareh Rajaei
- Bas Brinkhof
- Corine Vermeulen-Hangelbroek
- Cyril P. Landstra
- Dirk-Jan Cornelissen
- Elena Naumovska
- Esmée Dekker
- Evelien Rossenberg
- Ezra van der Wel
- Ferdy Lambregtse
- Lizanne Daleman
- Maaike Hanegraaf
- Maaike Nieveen
- Maarten Tol
- Maarten van Agen
- Michiel Nijhoff
- Natascha de Graaf
- Twan de Winter
- Yun Suk Chae
Islet group research
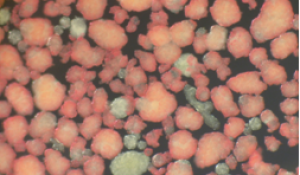
The insulin-producing beta cells in the Islets of Langerhans of the pancreas play a key role in all types of diabetes mellitus. The islets of Langerhans are the main focus of both clinical and basic research projects. The Islet group started in 2006 when a human islet isolation laboratory was established in the Leiden University Medical Center followed by a clinical islet transplantation program in 2007. This enabled the establishment of basic and clinical research programs involving human islet cells. Basic research focuses on human islet cell identity, islet survival and function, and strategies in order to generate new insulin-producing cells. Clinical research is focused on improvement of current human islet isolation and beta cell replacement therapy, and on assessment of islet function and damage in patients with severe beta cell failure (in particular type 1 diabetes). The following topics are key areas of research:
Human islet isolation and clinical beta-cell replacement therapy
Diabetes due to loss and/or failure of the insulin-producing beta cells (in particular type 1 diabetes, but also severe forms of chronic pancreatitis (cystic fibrosis), or pancreatectomy) requires administration of exogenous insulin and is usually associated with instable glycemic control compared to patients with substantial residual beta cell function. Patients with severe beta cell failure due to type 1 diabetes often develop this disease at a young age. Beta cell replacement is the only therapeutic modality to restore normal sugar levels without the risk of hypoglycemia side effects. In the LUMC beta cell replacement is an integrated program consisting of pancreas transplantation (since 1984) and islet transplantation (since 2007).
Our research focuses on improvement of human islet isolation and transplantation outcome. Areas of research include pancreas preservation strategies and new techniques to isolate human islets. Preclinical studies on human islets are performed to improve islet survival. And novel immunosuppressive regimes and peritransplant strategies are tested. In collaboration with the group of Aart van Apeldoorn (University of Maastricht) preclinical studies are performed using scaffolds in order to create alternative transplantation sites and improve islet function and survival. This work was also part of the Diabetes Cell Therapy Initiative, a Dutch consortium focused on improvement of islet transplantation, coordinated by our group.
Marten Engelse, Assistant Professor and Head Islet Isolation Laboratory
Françoise Carlotti, Associate Professor and Head Islet Research Laboratory
Dirk-Jan Cornelissen, Postdoc
Michiel Nijhoff, Endocrinologist
Maarten Tol, PhD student
Cyril Landstra, PhD student
Yun Suk Chae, PhD student
Esmay Hammink, PhD student
Eelco de Koning, Professor and Head Islet Group. Head Section of Diabetes and Clinical Director Islet Transplantation Program
Alternative sources of beta cells
Beta cell replacement therapy is an attractive treatment option for patients with beta cell failure but the procedure is limited to a small number of patients with severe beta cell failure due to the need for an alternative source of insulin-producing cells and the scarcity of organ donors.
In collaboration with the De Koning group at the Hubrecht Institute in Utrecht, we investigate the use of adult human pancreatic tissue for regenerative purposes. Human duct cells can be isolated from the islet-depleted pancreatic tissue after islet purification. These cells are an attractive source of islet progenitors as ductal tissue is involved in islet neogenesis in vivo. Two key issues that are relevant for clinical application need to be optimized: the maintenance and expansion of the adult pancreatic cells and the reprogramming of expanded cells towards functionally active beta cells.
Since 2017 our group coordinates the diabetes project in the Dutch consortium for regenerative medicine RegMedXB. The diabetes project in this consortium is focused on advancing beta-cell replacement therapy using human pluripotent stem cells as alternative cell source and immunoevasive devices in patients with severe beta-cell failure. Since 2020, our group takes part in the H2020 consortium ISLET that is dedicated to advancing innovative stem cell-based therapy for diabetes in Europe.
Since 2022 we are part of reNEW, an international consortium of three leading research institutions in Denmark, Australia and the Netherlands. The aim of renew is to create a new generation of innovative stem cell-based therapies to help transform the lives of people suffering from incurable diseases such as diabetes.
Françoise Carlotti, Associate Professor and Head Islet Research Laboratory
Marten Engelse, Assistant Professor and Head Islet Isolation Laboratory
Bahareh Rajaei, Postdoc
Bas Brinkhof, Postdoc
Elena Naumovska, Postdoc
Roxanna Hauck, PhD student
Eelco de Koning, Professor and Head Islet Group. Head Section of Diabetes and Clinical Director Islet Transplantation Program
Human islet-cell identity and function
The insulin producing beta cells are essential to maintain blood glucose levels within a narrow range. When the demand for insulin is chronically increased by physiological or pathological changes, beta cells can adapt by enhancing insulin secretion (increased function) and/or enhancing beta cell number (increased mass). Inadequate adaptation leads to the development of hyperglycemia and eventually to diabetes. Therefore, insight into the mechanisms and signaling pathways that control beta cell identity and adaptation to environmental stress conditions is important for developing therapies that can preserve or enhance functional beta-cell mass.
Our group takes part in the H2020 consortium ESPACE that is aiming to build a Human Cell Atlas of the Pancreas.
In addition we explore the function of residual beta cells in patients with type 1 diabetes and markers of beta cell dysfunction both in vitro and in vivo.
Françoise Carlotti, Associate Professor and Head Islet Research Laboratory
Amadeo Muñoz Garcia, Postdoc
Fransje Boot, PhD student
Miriam Paz-Barba, PhD student
Esmee Dekker, PhD student
Eelco de Koning, Professor and Head Islet Group. Head Section of Diabetes and Clinical Director Islet Transplantation Program
Other members of the Islet Group:
Corine Vermeulen-Hangelbroek, technician
Evelien Rossenberg, technician
Maarten van Agen, technician
Natascha de Graaf, technician
Maaike Nieveen, technician
Maaike Hanegraaf, technician
Lizanne Daleman, technician
Ferdy Lambregtse, technician
Anne de Leeuw, technician
Natasja de Jong, technician
Ezra van der Wel, technician
Esther Steeneveld, technician
Iris Claessen, technician
Saskia du Pré, Project Manager
RECENT KEY PUBLICATIONS:
- Fasting parameters for estimation of stimulated β-cell function in islet transplant recipients with or without basal insulin treatment. Uitbeijerse BS, Nijhoff MF, Sont JK, de Koning EJP. Am J Transplant. 2020 Jun 10.
- Advances in β-cell replacement therapy for the treatment of type 1 diabetes. Vantyghem MC, de Koning EJP, Pattou F, Rickels MR. Lancet. 2019 Oct 5;394(10205):1274-1285.
- Organoids from the Human Fetal and Adult Pancreas. Balak JRA*, Juksar J*, Carlotti F, Lo Nigro A, de Koning EJP. Curr Diab Rep. 2019 Dec 11;19(12):160.
- Tacrolimus-Induced BMP/SMAD Signaling Associates With Metabolic Stress-Activated FOXO1 to Trigger β-Cell Failure. Triñanes J, Ten Dijke P, Groen N, Hanegraaf M, Porrini E, Rodriguez-Rodriguez AE, Drachenberg C, Rabelink TJ, de Koning E, Carlotti F*, de Vries APJ*. Diabetes. 2020 Feb;69(2):193-204
- Highly efficient ex vivo lentiviral transduction of primary human pancreatic exocrine cells. Balak JRA, de Graaf N, Zaldumbide A, Rabelink TJ, Hoeben RC, de Koning EJP, Carlotti F. Sci Rep. 2019 Nov 1;9(1):15870.
- Expansion of Adult Human Pancreatic Tissue Yields Organoids Harboring Progenitor Cells with Endocrine Differentiation Potential. Loomans CJM*, Williams Giuliani N*, Balak J, Ringnalda F, van Gurp L, Huch M, Boj SF, Sato T, Kester L, de Sousa Lopes SMC, Roost MS, Bonner-Weir S, Engelse MA, Rabelink TJ, Heimberg H, Vries RGJ, van Oudenaarden A, Carlotti F, Clevers H, de Koning EJP. Stem Cell Reports. 2018 Mar 13;10(3):712-724.
- Pancreatic α-cell mass in obesity. Ellenbroek JH, Töns HAM, Hanegraaf MAJ, Rabelink TJ, Engelse MA, Carlotti F, de Koning EJP. Diabetes Obes Metab. 2017 Dec;19(12):1810-1813.
- Increased vimentin in human α- and β-cells in type 2 diabetes. Roefs MM*, Carlotti F*, Jones K, Wills H, Hamilton A, Verschoor M, Durkin JMW, Garcia-Perez L, Brereton MF, McCulloch L, Engelse MA, Johnson PRV, Hansen BC, Docherty K, de Koning EJP, Clark A. J Endocrinol. 2017 Jun;233(3):217-227.
- A Single-Cell Transcriptome Atlas of the Human Pancreas. Muraro MJ*, Dharmadhikari G*, Grün D, Groen N, Dielen T, Jansen E, van Gurp L, Engelse MA, Carlotti F, de Koning EJ*, van Oudenaarden A*. Cell Syst. 2016 Sep 28.
- Glycemic Stability Through Islet-After-Kidney Transplantation Using an Alemtuzumab-Based Induction Regimen and Long-Term Triple-Maintenance Immunosuppression. Nijhoff MF, Engelse MA, Dubbeld J, Braat AE, Ringers J, Roelen DL, van Erkel AR, Spijker HS, Bouwsma H, van der Boog PJ, de Fijter JW, Rabelink TJ, de Koning EJ. Am J Transplant. 2016 Jan;16(1):246-53.
- Loss of β-Cell Identity Occurs in Type 2 Diabetes and Is Associated With Islet Amyloid Deposits. Spijker HS, Song H, Ellenbroek JH, Roefs MM, Engelse MA, Bos E, Koster AJ, Rabelink TJ, Hansen BC, Clark A, Carlotti F, de Koning EJ. Diabetes. 2015 Aug;64(8):2928-38
ISLET GROUP IN THE MEDIA:
Television
2017 Dokters van Morgen (Dutch)
2015 Tijd voor Max (Dutch)
2014 RTL Toekomstmakers – Diabetes (Dutch)
2013 NTR – Over leven met ….diabetes (Dutch)
2007 TELEAC – Wetenschap is beterschap (Dutch)
Radio
2018 Nieuws en Co
Website videos
2016 Leiden University MOOC Clinical kidney transplantation – Lecture 2.7: Simultaneous kidney pancreas and islet transplantation (English)
2016 Leiden University MOOC MOOC Clinical kidney transplantation – Lecture 4.4: Late challenges after pancreas and islet transplantation (English)
2015 Bontius Stichting (LUMC) – Eilandjes transplantatie bij type 1 diabetes (Dutch)
2014 Ééndiabetes – Interview Eelco de Koning (Dutch)
2012 Diabetes Fonds – Stamcellen voor diabetes in kader van prijsvraag (Dutch)
Other news item
2019 Financieel Dagblad – Als niets meer helpt dan maar een maagverkleining
2019 nu.nl – Onderzoek naar diabetes type I moet spuiten insuline overbodig maken
2019 Margriet magazine – Onderzoek beta-cellen diabetes type I
2019 Diligentia – Natuurkundige Voordrachten 2018-2019, nieuwe reeks no. 97, uitgave Koninklijke Mij voor Natuurkunde ‘Diligentia’. (Dutch)
2015 LUMC – Dr. F. Gerritzen prijs voor Rianne Ellenbroek (Dutch)
2015 LUMC/ Bontrius stichting – Onderzoek naar celtherapie als behandeling van type 1 diabetes
2014 LUMC – LUMC ontvangt grote subsidies voor diabetesonderzoek (Dutch)
2014 Diapedia – Islet transplantation (English)
2012 Inaugural lecture Eelco de Koning (Dutch)
Former group members:
Ronald van der Sluis
Laura Paardekooper
Nathalie Groen (post-doc)
Floris Leenders (PhD student)
Javier Trinanes (post-doc)
Annemieke Tons (technician)
Bas Uitbeijerse, MD (PhD student)
Aniela Skrzypczyk (post-doc)
Cindy Loomans, PhD (post-doc)
Rianne Ellenbroek-den Doelder, PhD (PhD student and post-doc)
Siebe Spijker, MD (PhD student)
Maaike Roefs, MSc (PhD student)
Jeetindra Balak. MD (PhD student)
Nerys Williams, MSc (PhD student)
Matthias Roost, MSc (shared PhD student)
Leone Carlée (technician)
Tim Dielen (technician)
Jeroen Sijtsma (technician)
Merel M. Ruissen, MD (PhD student)
Jason Doppenberg, MSc (PhD student)
Anja Steffen, PhD (Postdoc)
Annina Roelofsen (Technician)
Ehsan Shokrollahi (Technician)
Diego S. Piani (Technician
Elisa van der Sar, MSc (Technician)